BIOMIMETIC DERMOID GRAFTS WITH ALLOGENIC BIOACTIVITY: AN INNOVATIVE APPROACH FOR HERNIA REPAIR IN BUFFALOES
DOI:
https://doi.org/10.56825/bufbu.2025.4445906Keywords:
Bubalus bubalis, buffaloes, dermoid graft, allogenic, hernia, laparotomy, herniorrhaphyAbstract
Hernia development is a common abdominal wall condition observed in calves, frequently manifesting in the umbilical region. This innovative biological dermoid scaffold is considered superior because of their inherent ability to combat infections through the release of antimicrobial peptides and non-complement fixing antibodies.
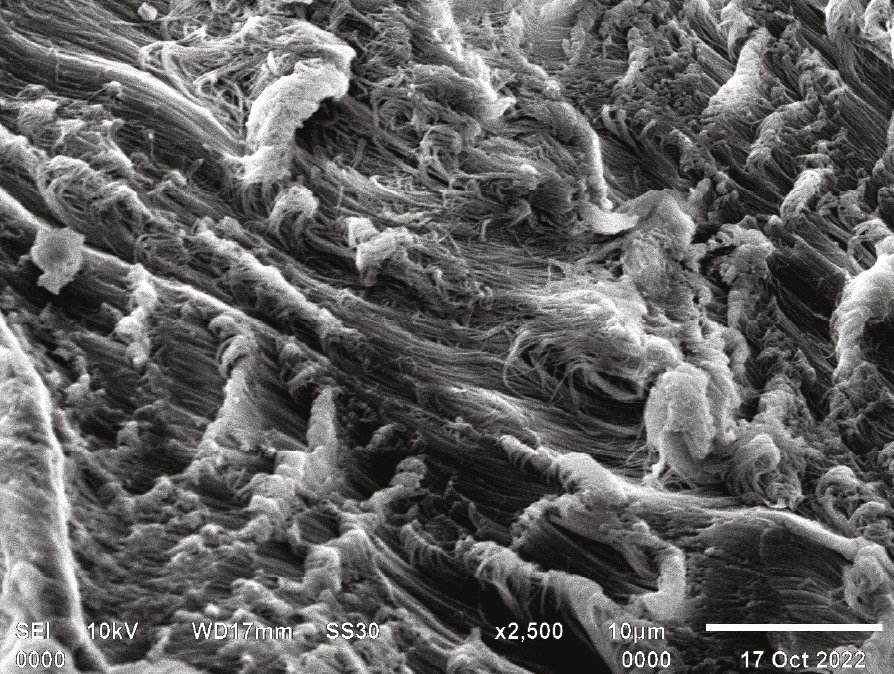
The Division of Surgery at ICAR-IVRI, Izatnagar, has pioneered the development of bioinspired-bioactive dermoid scaffolds, as an initiative aimed at addressing hernias in large animals. The in vitro evaluation of the scaffold included crucial parameters such as H and E staining, SEM evaluation, and scaffold-cell interaction. Histocompatibility, cyto-toxicity, cell attachment, and proliferation of the seeded scaffolds were assessed using DAPI staining, along with an examination of porosity and density.
All cases share a common history of a large swelling in the abdominal region. Physical examination, palpable hernial ring was identified followed by USG examination leading to the diagnosis of a large ventral hernia. Hematobiochemical analysis indicated a slight metabolic alkalosis, along with mild anaemia and azotaemia. Subsequent exploratory laparotomy was performed, to address the large abdominal defect, we decided to repair it using an allogenic dermoid graft in an overlaid fashion. Postoperative care included a 7-day course of antibiotics, analgesics, and antihistamines. All buffaloes in the study exhibited uneventful recovery, with no recurrence observed during the 5-month follow-up period.
No reports on treatment of large abdominal wall defects with dermoid graft reported, which prevent reoccurrence of hernia. This study marks for the first time, where we outline the successful closure of a hernia in clinical cases.
Downloads
Metrics
References
Abdin-Bey, M.R. and R.O. Ramadan. 2001. Retrospective study of hernias in goats. Scientific Journal of King Faisal University, 2(1): 1421-1425.
Aldridge, A. and J. Simson. 2001. Erosion and perforation of colon by synthetic mesh in a recurrent paracolostomy hernia. Hernia., 5(2): 110-112. DOI: https://doi.org/10.1007/s100290100007
Al-Sobayil, F.A. and A.F. Ahmed. 2007. Surgical treatment for different forms of hernias in sheep and goats. Journal of Veterinary Science, 8(2): 185-191. DOI: https://doi.org/10.4142/jvs.2007.8.2.185
Baylón, K., P. Rodríguez-Camarillo, A. Elías-Zúñiga, J.A. Díaz-Elizondo, R. Gilkerson and K. Lozano. 2017. Past, present and future of surgical meshes: A review. Membranes, 7(3): 47.
Bellows, C.F., D. Albo, D.H. Berger and S.S. Awad. 2007. Abdominal wall repair using human acellular dermis. Am. J. Surg., 194(2): 192-198. DOI: https://doi.org/10.1016/j.amjsurg.2006.11.012
Bhat, M.A., M.M.S. Zama, A.S. Batoo, M. Javaid, R. Pathak, A. Suvarna, M. Hoque, R. Singh and N. Sharma. 2015. Preparation and functional characterization of decellularized bovine tendon scaffolds for tendon tissue engineering. Am. J. Surg., 5(4): 921-926.
Doijode, V. 2019. Umbilical hernia in ruminant calves: A review. Pharma. Innov., 8(4): 164-167. Available on: https://www.thepharmajournal.com/archives/2019/vol8issue4/PartC/8-3-30-374.pdf
Elango, S., S. Perumalsamy, K. Ramachandran and K. Vadodaria. 2017. Mesh materials and hernia repair. Biomedicine (Taipei), 7(3): 16. DOI: https://doi.org/10.1051/bmdcn/2017070316
Eskandaros, M.S. and A.A. Darwish. 2017. Component separation technique versus inlay mesh technique in patients with large incisional hernia. Egyptian Journal of Surgery, 36(2): 145-151. DOI: https://doi.org/10.4103/1110-1121.204528
Falagas, M.E. and S.K. Kasiakou. 2005. Mesh-related infections after hernia repair surgery. Clin. Microbiol. Infect., 11(1): 3-8. DOI: https://doi.org/10.1111/j.1469-0691.2004.01014.x
Fang, F. and S.P. Lake. 2017. Experimental evaluation of multiscale tendon mechanics. J. Orthop. Res., 35(7): 1353-1365. DOI: https://doi.org/10.1002/jor.23488
Franz, M.G. 2008. The biology of hernia formation. Surg. Clin. North Am., 88(1): 1-15. DOI: https://doi.org/10.1016/j.suc.2007.10.007
Ghodbane, S.A. and M.G. Dunn. 2016. Physical and mechanical properties of cross-linked type I collagen scaffolds derived from bovine, porcine, and ovine tendons. J. Biomed. Mater. Res. A., 104(11): 2685-2692. DOI: https://doi.org/10.1002/jbm.a.35813
Hezbollahi, M., N.M. Shahri, M.M. Matin and R. Lari. 2013. Fabrication of a bioscaffold from bovine tendon for possible applications in tissue engineering. In Proceedings of the 13th Iranian Congress of Biochemistry and 5th International Congress of Biochemistry and Molecular Biology, Yazd, Iran.
Jaman, M.M., P. Mishra, M. Rahman and M.M. Alam. 2018. Clinical and laboratory investigation on the recurrence of the umbilical hernia after herniorrhaphy in bovine calves. Journal of the Bangladesh Agricultural University, 16(3): 464-470. DOI: https://doi.org/10.3329/jbau.v16i3.39418
Janet, J., S. Derbal, S. Durand-Fontanier, S. Bouvier, N. Christou, A. Fabre, F. Fredon, T. Rivaille, D. Valleix, M. Mathonnet and A. Taibi. 2021. C-reactive protein is a predictive factor for complications after incisional hernia repair using a biological mesh. Sci. Rep., 11(1): 1-8. DOI: https://doi.org/10.1038/s41598-021-83663-6
Jansen, P.L., P.R. Mertens, U. Klinge and V. Schumpelick. 2004. The biology of hernia formation. Surgery, 136(1): 1-4. DOI: https://doi.org/10.1016/j.surg.2004.01.004
Lee, C.H., A. Singla and Y. Lee. 2001. Biomedical applications of collagen. Int. J. Pharm., 221(1-2): 1-22. DOI: https://doi.org/10.1016/s0378-5173(01)00691-3
Liu, W., Y. Xie, Y. Zheng, W. He, K. Qiao and H. Meng. 2021. Regulatory science for hernia mesh: Current status and future perspectives. Bioact. Mater., 6(2): 420-432. DOI: https://doi.org/10.1016/j.bioactmat.2020.08.021
Mohsina, A., P. Tamilmahan, D.D. Mathew, V. Remya, N.A. Ravindran, N. Kumar, S.K. Maiti, K. Karthik and M.H. Vasanthachar. 2014. Biomaterials for hernia repair in animals: A review. Adv. Anim. Vet. Sci., 2(4S): 48-54. DOI: https://doi.org/10.14737/journal.aavs/2014/2.4s.48.54
Ober, C., A. Muste, L. Oana, N. Mateş, F. Beteg and S. Vereş. 2008. Using of prosthetic biomaterials in large animals: Modern concepts about abdominal wall defects approach. J. Cent. Eur. Agric., 9(3): 575-580. DOI: https://doi.org/10.5513/jcea.v9i3.707
Pratschke, K. 2002. Management of hernias and ruptures in small animals. In Pract., 24(10): 570-581. DOI: https://doi.org/10.1136/inpract.24.10.570
Robinson, T.N., J.H. Clarke, J. Schoen and M.D. Walsh. 2005. Major mesh-related complications following hernia repair: Events reported to the food and drug administration. Surg. Endosc., 19(12): 1556-1560. DOI: https://doi.org/10.1007/s00464-005-0120-y
Sackett, S.D., D.M. Tremmel, F. Ma, A.K. Feeney, R.M. Maguire, M.E. Brown, Y. Zhou, X. Li, C. O’Brien, L. Li and W.J. Burlingham. 2018. Extracellular matrix scaffold and hydrogel derived from decellularized and delipidized human pancreas. Sci. Rep., 8(1): 1-16. DOI: https://doi.org/10.1038/s41598-018-28857-1
See, C.W., T. Kim and D. Zhu. 2020. Hernia mesh and hernia repair: A review. En. Regen., 1(1): 19-33. DOI: https://doi.org/10.1016/j.engreg.2020.05.002
Silvipriya, K.S., K.K. Kumar, A.R. Bhat, B.D. Kumar, A. John and P. Lakshmanan. 2015. Collagen: Animal sources and biomedical application. J. Appl. Pharm. Sci., 5(3): 123-127. DOI: https://doi.org/10.7324/JAPS.2015.50322
Zhou, S., B. Yuan, W. Huang, Y. Tang and X. Chen. 2021. Preparation and biological characteristics of a bovine acellular tendon fiber material. J. Biomed. Mater. Res. A., 109(10): 1931-1941. DOI: https://doi.org/10.1002/jbm.a.37185
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2025 Buffalo Bulletin

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.







.png)